|
Wisdom Teeth
What are wisdom teeth?
The information presented on this site is of personal opinion and consequently is slanted and biased and not based on proper scientific research. The information presented is NOT written by a dental expert. Further the information presented has NOT been subjected to peer review by experts to verify accuracy and data integrity.
Wisdom teeth are third molars that usually appear in the late teens and early 20s. It is also possible they will not erupt. Wisdom teeth are the last adult teeth to come through. There are usually four of them, right at the back of the mouth.
Around 25% of people will not have at least one of of the usual four wisdom teeth. If a wisdom tooth is going to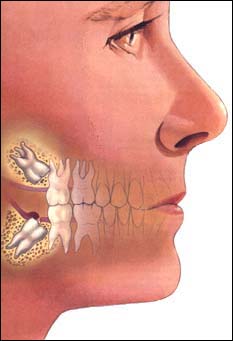 erupt and emerge it will typically do so by 25 years of age. [5] erupt and emerge it will typically do so by 25 years of age. [5]
What are impacted wisdom teeth?
Sometimes, wisdom teeth don’t emerge and come through the gum properly. This usually happens when there isn’t enough space, or when the teeth are growing in the wrong direction. If wisdom teeth don't erupt and emerge properly, they’re called impacted wisdom teeth.
A wisdom tooth is impacted when there is lack of space in the jaw, obstruction by another adjacent second molar which blocks the wisdom tooth, and/or the wisdom tooth develops in an abnormal position as in it comes in at an awkward angle. [5]
Studies have shown that the chances a person has at least one impacted wisdom tooth is as high as approximately 73%. [5]
What is surgery to remove wisdom teeth?
An operation to remove wisdom teeth involves making a small cut in the gum, separating the tooth from the jawbone and taking it out of the mouth. The teeth might be taken out whole or in small pieces.
Who should have this operation?
Taking out wisdom teeth is one of the most common operations in developed countries. But some people don’t need their wisdom teeth removed, even if the teeth are impacted. In order to properly assess if a wisdom tooth should or should not be removed an x-ray taken by a dentist or other experienced clinician is needed.
Guidelines from the (British) National Institute for Health and Clinical Excellence (NICE) and Scottish Intercollegiate Guidelines Network (SIGN), say that an impacted wisdom tooth should only be taken out if it’s causing problems as in if it has associated pathology or there is some other indication for it's removal. [2, 3]
Reasons for Wisdom Teeth Removal Associated with Pathology / Problems:
• Periodontal disease (gum disease)
• Recurrent pericoronitis (multiple episodes of infection of the gum around a wisdom tooth)
• Abscess, cellulitis, and osteomyelitis (infection spread from wisdom tooth into surrounding tissues)
• Untreatable pulpal and/or periapical pathology
• A cavity in a tooth a dentist can't treat as in an unrestorable carie (decay) in a wisdom tooth or adjacent tooth when the cavity in the adjacent tooth can't be properly treated without removal of the wisdom tooth
• Disease of follicles including a cyst (a sac filled with fluid) or tumor.
• Root, bone, and/or crown breakdown next to/(or to) a wisdom tooth also known as internal/external resorption (which includes damage to a neighbouring tooth)
• Fracture of a wisdom tooth
• When a wisdom tooth is involved in a fracture line
• When a wisdom tooth is involved in or within the field of tumor resection
If one of these problems is present the following may develop
• Pain or tenderness in the gums or jawbone
• Bad breath
• Redness or swelling in the gums
• An unpleasant taste in the mouth
• Headaches or jaw ache.
This image is from http://www.flickr.com/photos/jaredkse/5373551355/ and by Jared Krause. It is used with permission.
Other Indications for a Wisdom Tooth to be Removed
• For the use of a wisdom tooth for autogenous transplantation into another area such as a first molar socket.
• When specific medical conditions or surgical conditions are present and the risk of keeping the wisdom tooth is potentially more dangerous than the complications arising from removing the wisdom tooth (such as organ transplantation, chemotherapy, alloplastic implants, cardiac valvular disease or radiotherapy).
• When there is atypical pain from an unerupted wisdom tooth and removing the wisdom tooth can remove the possibility that the atypical pain is not from muscle dysfunction or the temporomandibular joint.
• When a unerupted wisdom tooth or partially erupted wisdom tooth is close to the alveolar surface prior to a planned implant or denture construction.
• When an adjacent tooth's (second molar) eruption is prevented by a wisdom tooth.
• When a wisdom tooth is in the way of surgery such as orthognathic surgery or reconstructive jaw surgery.
• In patients who have certain risks due to their lifestyle or occupation that may prevent them from easy access to dental treatment. This may include patients who have very little money/ plan to have very little money in the future which may prevent them from being able to afford treatment for a problematic wisdom tooth that may arise.
• When it is necessary to remove at least one wisdom tooth, consideration should be given that removing another wisdom tooth or wisdom teeth during this time may have less risk than keeping the other wisdom tooth or wisdom teeth which could potentially require additional pain, anesthesia, surgery, missing school/work, recovery, medications, and cost in the future.
If wisdom teeth are not causing problems and there is no other indication for removal, it may be best to keep wisdom teeth and avoid the risks of surgery. Sometimes, as wisdom teeth come through, gums may feel sore or tender for a while. This is normal, and isn’t usually a reason for having them removed. If one or two wisdom teeth need to be extracted, it doesn’t necessarily mean that all wisdom teeth need to be removed and taken out.
The American Association of Oral and Maxillofacial Surgeons (AAOMS) also lists a few additional indications for removal of wisdom teeth in addition to what is discussed in the guidelines from SIGN and NICE as stated above. [26, 52]
• To facilitate prosthetic rehabilitation
• To facilitate the management or limit progression of periodontal disease
• When a wisdom tooth is in an ectopic position (off normal position/eruption path)
• To facilitate orthodontic tooth movement and promote dental stability
• When orthodontic abnormalities are present (such as arch length/tooth size discrepancies)
• When there is insufficient space to accommodate an erupting wisdom tooth or wisdom teeth
In addition although not listed in any of the guidelines above partially erupted wisdom teeth and horizontally impacted wisdom teeth deserve consideration for extraction. See the controversy page for further discussion. [4, 19, 25, 52, 53]
In the cases of healthy impacted wisdom teeth the decision to extract or not is ultimately up to the patient with valuable input from their dentist and/or oral surgeon and/or other medical professionals. The guidelines above may be dated and potentially have changed.

This image is from http://www.flickr.com/photos/amymessere/3307505841/ and by Amy Messere. It is used with permission and has a Creative Commons license.
Do wisdom teeth cause crowding?
Wisdom teeth crowding refers to the theory that erupting wisdom teeth push and shift the anterior (as in the 6 lower front teeth) forward and thus cause their crowding. It has been shown that wisdom teeth do not cause crowding. Even so many oral surgeons still continue to recommend the removal of lower wisdom teeth to prevent crowding. [4, 6, 7]
There have been many studies performed to investigate the role wisdom teeth may play in late lower incisor crowding. Most of the studies found minimal or no effects as in no statistically significant difference of crowding in the lower dental arch, when comparing subjects who never had wisdom teeth develop, who had wisdom teeth removed, and who have wisdom teeth. Hence it is recommended that removing wisdom teeth should be based on other reasons and not based soley on the possibility that wisdom teeth could in the future cause lower incisor crowding. [4, 6]
A 40 year follow up study of 18 participants in Sweden showed that there is increased crowding of the anterior teeth as one ages but this occured in both people with wisdom teeth and people without wisdom teeth. [50, 51]
See https://blog.teethremoval.com/do-wisdom-teeth-cause-crowding/ for additional information.
Is there an ideal age to have wisdom teeth removed?
Studies have looked at how the age a person has a wisdom tooth or wisdom teeth removed affects their postoperative recovery and amount of complications developed. For example, the American Association of Oral and Maxillofacial Surgeons' (AAOMS) Age-Related Third Molar Study showed that patients over 25 were statistically significantly more likely to experience a complication compared with their counterparts under age 25. Other evidence from other studies also tends to show an increase in age is associated with an increase in a complication occuring after wisdom teeth removal and increased difficulty of extraction. [4, 13, 14, 21, 24, 54]
Even so the results of some of these age related studies may be misleading. In the study mentioned above, 93.9% of the people in the study were over the age of 25 making comparisons to those under 25 potentially not valid. In fact, in that study and another also by AAOMS, both appearing in the Journal of Oral and Maxillofacial Surgery, the data showed the highest risk of complications occuring after wisdom teeth removal is in those aged 25 to 35 years old. One study was published in 2007 and looked at 4,004 patients and the other study was published in 1985 and looked at 9,547 patients. [14, 18, 19]
With an increase in age there tends to be an increase in the health risk factors (such as smoking, pathology present, oral contraceptive use, the surgeon's skill and experience, and the type of impaction) which then influence postoperative recovery. Thus with older age delayed healing and more pain could occur after surgery. [4, 20, 48] Further, when a patient is younger the roots of the wisdom teeth are not as fully developed as later age. Some studies have suggested that when the roots are more fully developed it is more possible for nerve injuries to occur. In addition at older age, there may be a decrease in nerve regeneration and neuronal plasticity. [55, 56] One study reviewed various complications that may occur after wisdom teeth removal and found that in general as one ages the different complications looked at (sinus complications, mandibular fracture, tuberosity fracture, infections, periodontal complications, nerve damage, and temporomandibular joint problems) are more likely to occur (or cause more problems). [58]
Even so, removing wisdom teeth soley on the basis that in the future (due to increasing age) extraction will result in greater complications and morbidity is not justified. [4]
What will happen without surgery to remove wisdom teeth?
If impacted wisdom teeth are causing you problems, it’s hard to know what will happen if they are not extracted. There isn’t much research, but most experts agree that it’s best to take wisdom teeth out that are causing problems. If these wisdom teeth with problems are kept mild infections may come and go which could require antibiotics. Serious infections are rare, but can be dangerous. People with infected wisdom teeth can have high temperature and swelling in the their mouth which could potentially block their airways. An impacted wisdom tooth may damage nearby teeth and bone. Cysts (a sac filled with fluid) and tumors around the root of the impacted wisdom tooth can develop.
If wisdom teeth are impacted but aren’t causing problems and there is no other indication for removal, removing those wisdom teeth may do more harm than good. But the research on wisdom teeth isn’t very good, so it’s hard to say for certain what will happen.
• Symptoms may never develop. Many impacted wisdom teeth never cause problems.
• Impacted wisdom teeth may eventually emerge normally.
• On the other hand, problems in the future, such as an infection, a cavity, or gum disease can arise.
Thus in those patients who do not have surgery to remove wisdom teeth and have at least one wisdom tooth, (beyond their late teenage years) they should have a dentist or other experienced clinician exam the wisdom tooth or wisdom teeth at least every 2 years and preferably every 12 months to 18 months. X-rays should also be regularly performed with the interval between examinations determined by the individual needs of the patient and assessment by the dental team. This will aid in the preventation of developing symptoms, damage, and disease that could potentially occur. [8, 9] Following an active surveillance follow-up program is advised over only performing follow-up when symptoms or disease present. This is because symptoms can be a late finding in the disease process of already progressing disease. [57]
Retaining wisdom teeth and not having surgery can in some cases, potentially be more costly than having surgery and having wisdom teeth removed. It is possible to perform a cost analysis as suggested in [57]; however, such an analysis can be difficult because of the unknown. See https://blog.teethremoval.com/the-costs-associated-with-third-molars-wisdom-teeth/ for further discussion.
Learn more in depth and detail about the risks of keeping wisdom teeth / reasons for their removal.
Are dental x-rays of wisdom teeth safe?
Most commonly wisdom teeth are looked at with a panoramic x-ray also called a panorex. This allows for one to determine if a wisdom tooth is impacted. During a panoramic x-ray a patient will bite down on a tool that allows the person performing the x-ray to properly position the patient's head. The person having the panoramic x-ray will then need to hold still for 10 to 20 seconds while the x-ray machine is rotated. This produces a single large image of the teeth and jaws which is either displayed digitally on a computer or on traditional x-ray film. [10]
The average person in the U.S. recieves an effective dose of somewhere between about 3 millisieverts (mSv) and 6.2 millisieverts (mSv) per year or roughly between 0.00833 mSv and 0.01722 mSv per day from naturally occuring background radiation from cosmic radiation in outer space and radioactive materials. The expected radiation exposure from a having a panoramic x-ray ranges from 0.0047 mSv to 0.0149 mSv (depending on the machine). This means having a single panoramic x-ray done is comparable to what would be received by the average person living in the U.S. over a period of roughly less than 1 day to 2 days from naturally occuring background radiation. [11, 12, 28]
It has been found that a digital panoramic x-ray tends to have lower effective radiation doses when compared to analogue (x-ray film) panoramic x-rays. [12]
A cone beam CT-scan (CBCT) may also be considered to provide a three-dimensional (3D) view of the anatomy instead of a two-dimensional (2D) view provided by a panoramic x-ray. A cone beam CT-scan (CBCT) has an expected radiation exposure ranging from 0.087 mSv to 0.206 mSv (depending on the machine). This means having a single cone beam CT-scan (CBCT) done is comparable to what would be received by the average person living in the U.S. over a period of roughly 5 to 25 days from naturally occuring background radiation. [27]
The more radiation exposure a person receives, the greater the risk of cancer occuring. The thyroid and other organs can absorb radiation through external exposure from an x-ray machine and hence when receiving a dental x-ray. Radiation exposure does increase risk of thyroid cancer, and the risk increases with the amount of radiation exposure. The developing thyroid is especially susceptible to radiation. Children exposed to radiation are at an increased risk of developing radiation absorption in the thyroid. Cancer caused by radiation generally takes many years to appear. Thyroid cancer is one of the most survived types of cancers and in some cases does not need to be treated. For prospective, in the U.S. roughly 48,000 people are diagnosed with thyroid cancer each year and 1,740 people die from thyroid cancer each year. [29, 30, 32, 35, 49]
The American Dental Association says when a dental x-ray is taken a leaded apron can be placed over the torso to minimize radiation exposure to the abdomen and chest. In addition, a leaded thyroid collar can be used to minimize radiation exposure to the thyroid. [31]
In one study in 2010, that looked at 313 thyroid cancer patients (primary from Kuwait and also Arab countries and Southeast Asia - median age 35 {women}- and 38 {men}) 104 of these patients had a dental x-ray, and 57 patients who had a dental x-ray but did not have thyroid cancer served as control, where as 255 patients who did not have a dental x-ray and did not have thryoid cancer also served as control. A two times greater increased risk of developing thyroid cancer was found in those who had a dental x-ray (higher odds ratio=2.1, 95% confidence interval 1.4-31). [32]
In one study in 2008, that looked at breast cancer in women (U.S. born - Los Angeles County - diagnosed with breast cancer between 20 and 49 years) there were 1,117 women in the study that reported always wearing a lead apron and 112 women which did not always wear a lead apron before the age of 20 when having a dental x-ray. Those women who did not always wear a lead apron during dental x-rays before the age of 20 had an increased risk of developing breast cancer. (higher odds ratio=1.81, 95% confidence interval 0.95-3.42). [33]
Radiological examinations are to be used when there is a likely demonstrable clinical need in which the benefits of radiological examination likely outweigh the risks of radiation exposure. Cone beam CT should be used instead of panoramic x-ray (or in addition) if it is likely that clinically useful information will be obtained.
Can removing wisdom teeth cause a change in facial appearance?
It may be possible to have a change in facial appearance after wisdom teeth are extracted although not accepted by all in the field. The jaw structure and facial features could become more well defined after wisdom teeth removal. The physical lack of wisdom teeth after their extraction results in a lack of bone which supports the cheeks and muscles. After some time the muscular forces may undergo changes which can alter facial appearance. Of course beauty is in the eye of the beholder and after time this facial change (if even possible which again is not recognized as even being able to occur by all in the field) could potentially be looked on as negative by some. [34]
What can behavioral science tell us about the decision to extract or not to extract wisdom teeth?
Let's be honest, at the end of the day when evaluating the potential benefits and harms to having healthy impacted wisdom teeth removed or not removed it really is a quantity of life issue. This means the question are you asking yourself is if I do have my wisdom teeth removed today will it make me live longer in the future (or not). Don't led be astray. The probablity of dying from simply having wisdom teeth appears to be quite low. Even so, people have died from a problematic wisdom tooth. Unfortunately there is absolutely no data and clinical studies performed which can demonstrate whether or not having healthy impacted wisdom teeth removed at a young age will or will not lead to a longer life. (The hope is clearly that it will). Until the theory is put to the test the quantity of life issue when looked at from removing healthy impacted wisdom teeth in young adults will not be resolved. Even if the theory turns out to be true then what? [35]
Well, then the issue really becomes a quality of life issue and not quantity of life issue. It is well known from case descriptions and research studies some of which are outlined on the complications page that long term permanent risks are real and can be quite life altering and serious. It may be that the potential harms outweigh the potential benefits or the other way around (which also needs to be put further to the test of clinical studies).
There are numerous behavioral science techniques particularly from the field of behavioral economics which can be applied to the decision to extract or not to extract healthy impacted wisdom teeth: [36]
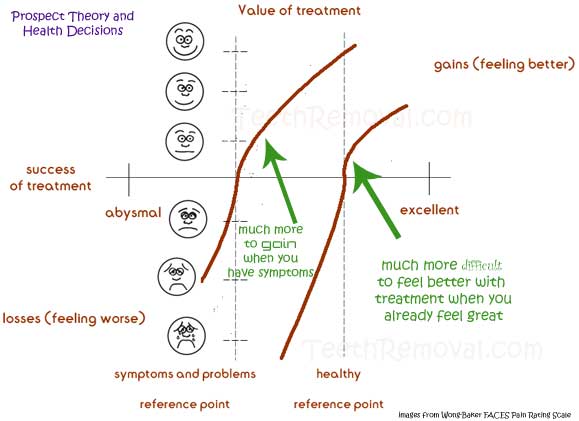
1) We do know from the work of Daniel Kahneman and Amos Tversky the theory of Prospect theory where people value risks (gains and losses) relative to some reference point. A young healthy adult with no symptoms more than likely values the outcome in terms of how they feel and not in terms of their potential life expectancy. Therefore this young healthy adult with no symptoms has a lot more to lose (in terms of harm) particularly when people have a tendency to prefer avoiding losses (becoming injured and/or sick) rather than acquiring gains (getting better). Think having my healthy impacted wisdom teeth removed will likely increase the length of my life. No! Your reference point is most likely how you feel not your life expectancy. [37, 45]
2) We know that people follow the bandwadgon effect where people are driven by social norms and what others do. People merely follow and do things that others follow and do. Think my friends are having healthy impacted wisdom teeth removed so I should to. No! Don't be driven by what other people around you are doing they may all be wrong (or right). [38, 39]
3) We know people tend to the follow the status quo and hence there is status quo bias where people often are not pro-active and prefer the default. Think my parents had their healthy impacted teeth removed so I should to. No! Your parents and their physicians may have been following health outcomes that were not ever put to any statistical test. [40]
4) We know that people tend to think their own stock portfolio can beat the stock market overall when this is absolutely impossible. This gets at the root of the issues of the better-than-average effects and judgmental overconfidence. The classic study is the 1981 survey of automobile drivers in which 90% of U.S. drivers in the study described themselves as above average drivers. Think my chance of having a complication from wisdom teeth removal knowing the risks is lower than everybody else's risk. No! Your risk is the same as everybody else's unless you have some underlying medical condition, problem, and/or anatomical variation that would make it otherwise. [42, 43, 44]
What are the potential uses of wisdom teeth?
You should also understand that research suggests stem cells can be harvested from wisdom teeth. Therefore, if you elect to have one or more wisdom teeth removed you may want to have the stem cells isolated and saved for potential later use. See the blog post https://blog.teethremoval.com/storing-wisdom-teeth-stem-cells/ for more information on possible storage services to consider.
Is there a wisdom teeth conspiracy?
Unfortunately it may even be possible for an implantable microchip to be put into a wisdom tooth extraction socket or other area of the mouth during wisdom teeth surgery. These microchips could potentially be used to track location and listen to conversations. This is extremely unlikely and extremely doubtful that it is currently occuring. See https://blog.teethremoval.com/wisdom-teeth-conspiracy-electronic-eavesdropping-device/ for additional information.
Updated October 14, 2019
References
1. Removing Wisdom Teeth. Clinical Evidence, the British Medical Journal. Written September 2006.
2. National Institute For Health and Clinical Evidence. Guidance of the Extraction of Wisdom Teeth. March 2000.
3. Scottish Intercollegiate Guidelines Network. Management of Unerupted and Impacted Third Molar Teeth.
September 1999.
4. S Kandasamy and DJ Rinchuse. The wisdom behind third molar extractions. Australian Dental Journal. 54. pages 284-292. 2009. http://onlinelibrary.wiley.com/doi/10.1111/j.1834-7819.2009.01152.x/abstract
5. Current Clinical Practice and Parameters of Care: The Management of Patients with Third Molar Teeth. Faculty of Dental Surgery. The Royal College of Surgeons of England. London. September 1997.
6. Šidlauskas Antanas and Trakinienė Giedrė. Effect of the lower third molars on the lower dental arch crowding. Stomatologija, Baltic Dental and Maxillofacial Journal. vol. 8. no. 3. pages 80-84. 2006.
7. H. Ryan Kazemi. DMD. The Wise Guide to Wisdom Teeth Extraction: Making Engaged Decisions about Your Wisdom Teeth Extraction. 2010. Licensed under Creative Commons Attribution 3.0 U.S. License.
8. Thomas B. Dodson and Srinivas M. Susarla. Impacted Wisdom Teeth. Search date July 2009. Clinical Evidence. 2010. 04:1302. pages 1- 17.
9. J. W. Friedman FRIEDMAN RESPONDS Am J Public Health, April 1, 2008; 98(4):582-582.
10. H. Ryan Kazemi. DMD. Exposure to Dental X-rays Raises Some Questions Regarding Its Safety.
December 29, 2010. https://www.facialart.com/2010/12/exposure-to-dental-x-rays-raise-some-questions-regarding-its-safety-bethesda-dentistry/ Accessed February 3, 2011.
11. Radiation Exposure in X-ray and CT Examinations. http://www.radiologyinfo.org/en/safety/index.cfm?pg=sfty_xray Accessed February 3, 2011.
12. F Gijbels and et. al. Dosimetry of digital panoramic imaging. Part I: patient exposure. Dentomaxillofacial Radiology. vol. 34. pages 145–149. 2005.
13. American Association of Oral and Maxillofacial Surgeons. White Paper on Third Molar Data.
Written March 2007.
14. Sung-Kiang Chuang, David H. Perrott, and Thomas B. Dodson. Age as a Risk Factor for Third Molar Surgery Complications. J Oral Maxillofac Surg. vol. 65. issue 9. pages 1685-1692. 2007.
15.
Ceib Phillips and et. al. Risk Factors Associated With Prolonged Recovery and Delayed Healing After Third Molar Surgery. J Oral Maxillofac Surg. vol. 61. issue 12. pages 1436-1448. 2003.
16. Chi H. Bui and et. al. Types, Frequencies, and Risk Factors for Complications After Third Molar Extraction. J Oral Maxillofac Surg. vol. 61. issue 12. pages 1379-1389. 2003.
17. Zaid H. Baqain and et. al. Frequency Estimates and Risk Factors for Postoperative Morbidity After Third
Molar Removal: A Prospective Cohort Study. J Oral Maxillofac Surg. vol. 66. issue 11. pages 2276-2283. 2008.
18. Thomas P. Osborn and et. al. A Prospective Study of Complications Related to Mandibular Third Molar Surgery. J Oral Maxillofac Surg. vol. 43. issue 10. pages 767-769. 1985.
19. Friedman JW. The prophylactic extraction of third molars: a public health hazard. Am J. Public Health. 2007. 97. pages 1554-1559.
20. American Association of Oral and Maxillofacial Surgeons. Third Molar Multidiscplinary Conference. October 19, 2010.
21. T. Renton, N. Smeeton, and M. McGurk. Factors predictive of difficulty of mandibular third molar surgery. British Dental Journal. vol. 190. no. 11. June 9 2001.
22. Thomas B. Dodson. Response to APHA C3: Oppostion to Prophylactic Removal of Third Molars. October 26, 2008.
23. Jay W. Friedman and Scott M. Presson. Wisdom tooth extraction in perspective. Dental Abstracts. vol. 55. issue 5. pages 228-229. 2010.
24. Ceib Phillips. Recovery after third-molar surgery: The effects of age and sex.
American Journal of Orthodontics and Dentofacial Orthopedics. vol. 138. issue 6. 700e1-700e8. December 2010.
25. Bertha Luk and et al. Prophylactic Extraction of Asymptomatic Third Molars to Prevent Periondontal Pathology: An Evidence Based Study.
Community Dentistry DEN207Y. University of Toronto. April 8, 2010.
26. Statement by the American Association of Oral and Maxillofacial Surgeons Concerning the Management of Selected Clinical Conditions and Associated Clinical Procedures. The Management of Impacted Third Molar Teeth. March 2010.
27. S Kapila, RS Conley, and WE Harrell Jr. The current status of cone beam computed tomography imaging in orthodontics. Dentomaxillofacial Radiology. vol. 40. pages 24–34. 2011.
28. United States Environment Protection Agency. Radiation Doses in Perspective. March 24, 2011.
29. Dr. Otis Webb Brawley. Does radiation from dental X-rays cause thyroid cancer? March 20, 2011. http://thechart.blogs.cnn.com/2011/03/30/does-radiation-from-dental-x-rays-cause-thyroid-cancer/ Accessed April 23, 2011.
30. United States Environment Protection Agency. Radiation: Risks and Realities. May 2007.
31. American Dental Association. X-Rays (Radiography). https://www.ada.org/en/member-center/oral-health-topics/x-rays Accessed April 23, 2011.
32. Anjum Memon and et al. Dental x-rays and the risk of thyroid cancer: A case-control study. Acta Oncologica. vol. 49. pages 447–453. 2010.
33. Huiyan Ma and et al. Low-dose medical radiation exposure and breast cancer risk in women under age 50 years overall and by estrogen and progesterone receptor status: results from a case–control and a case–case comparison. Breast Cancer Res Treat. vol. 109. pages 77–90. 2008.
34. Mark Burhenne DDS. Can Wisdom Teeth Surgery Cause a Thinning of the Face? August 12, 2010. https://askthedentist.com/can-wisdom-teeth-surgery-cause-a-narrowing-of-the-face/ Accessed May 20, 2011.
35. H. Gilbert Welch, Lisa M. Schwartz, and Steven Woloshin. Overdiagnosed: Making People Sick in the Pursuit of Health. Beacon Press. 2011.
36. Kevin P. Weinfurt. Value of High-Cost Cancer Care: A Behavioral Science Perspective. Journal of Clinical Oncology. vol. 25. no. 2. pages 223-227. 2007.
37. Kahneman, Daniel, and Amos Tversky. Prospect Theory: An Analysis of Decision under Risk. Econometrica. XLVII. pages 263-291. 1979.
38. Rao, Anand S. Behavioral Economics: Implications for an Aging Population's Wealth & Health Decisions. Diamond Management and Technology Consultants. The Second National Predictive Modeling Summit. Presented September 23, 2008 Washington, D.C.
39. Thaler, Richard H. & Sunstein, Cass R. Nudge: Improving Decisions About Health, Wealth, and Happiness. Yale University Press. 2008.
40. Samuelson, W. & R. J. Zeckhauser. Status quo bias in decision making. Journal of Risk and Uncertainty. 1. pages 7-59. 1998.
41. This website's owner paper. Using Behavioral Economics to Bring about Diet and Food Consumption Change. https://blog.teethremoval.com/using-behavioral-economics-to-bring-about-diet-and-food-consumption-change/ May 2009.
42. William J. Bernstein. The Four Pillars of Investing: Lessons for Building a Winning Portfolio. McGraw-Hill. 2010.
43. Richard P. Larrick, Katherine A. Burson, Jack B. Soll. Social comparison and confidence: When thinking you're better than average predicts overconfidence (and when it does not). Organizational Behavior and Human Decision Processes. vol. 102. pages 76-94. 2007.
44. Ola Svenson. Are We All Less Risky and More Skillful Than Our Fellow Drivers? Acta Psychologica. vol. 47. pages 143- 148. 1981.
45.
Alan Schwartz, Julie Goldberg, and Gordon Hazen. Prospect theory, reference points, and health decisions. Judgement and Decision Making. vol. 3. no. 2. pages 174-180. February 2008.
46. Marilyn J. Hockenberry and David Wilson. Wong's Essentials of Pediatric Nursing. 8th Edition. Mosby. St. Louis: 2009.
47. American Dental Association Council on Scientific Affairs. The use of dental radiographs. Update and recommendations. JADA. vol. 137. pages 1304-1312. September 2006.
48. Sanjivan Kandasamy. Evaluation and management of asymptomatic third molars: Watchful monitoring is a low-risk alternative to extraction. American Journal of Orthodontics and Dentofacial Orthopedics. Vol. 140. Issue 1.
pages 11-17. July 2011.
49. National Cancer Institute. Thyroid Cancer. https://www.cancer.gov/types/thyroid Accessed July 20, 2011.
50. Nokolasos, Tsiopas, Maria Nilner, Lars Bondemark, and Krister Bjerklin. A 40 years follow-up of dental arch dimensions and incisor irregularity in adults. The European Journal of Orthodontics Advance Access published October 19, 2011.
51. Dentistry.co.uk. Jaws shrink with age and impact on teeth. November 7, 2011.
52. AAOMS Response to Wisdom of Having That Tooth Removed. https://blog.teethremoval.com/wisdom-of-having-that-tooth-removed-aaoms-response/November 13, 2011.
53. Do I Really Need to Remove My Wisdom Tooth? https://blog.teethremoval.com/do-i-really-need-to-remove-my-wisdom-teeth/ November 2, 2011.
54. Q. B. Zhang and Z. Q. Zhang. Early extraction: a silver bullet to avoid nerve injury in lower third molar removal?
The International Journal of Oral and Maxillofacial Surgery. 2012.
55. AAOMS. Advocacy White Paper on Evidence Based Third Molar Surgery
56. Elena Queral-Gody, Eduard Valmaseda-Castellon, Leonardo Berini-Aytes, and Cosme Gay-Escoda, "Incidence and evolution of inferior alveolar nerve lesions following lower third molar extractions," Oral Surgery, Oral medicine, Oral Pathology, Oral Radiology and Endodontics, vol. 99 pp. 259-264, 2005
57. Thomas B. Dodson, Ira D. Cheifetz, William J. Nelson, and Louis K. Rafetto, "Summary of hte Proceedings of the Third Molar Multidisciplinary Conference," Journal of Oral and Maxillofacial Surgery, vol. 70, supplement 1, pp. 66-69, 2012.
58. M. Anthony Pogrel. What Is the Effect of Timing of Removal on the Incidence and Severity of Complications? Journal of Oral and Maxillofacial Surgery vol. 70, supplement 1, pp. S37-S40, 2012.
|